Job Search
SimplyHired.com is a job search engine that covers the largest jobs database on the planet and contains over 3.6m jobs currently. It looks like Google for job search.
Yahoo! releases My Web
This a response to Google's My Search History. Again, the search wars are head-to-head and there is no clear winner yet although Google seems a bit more inventive.
(via Geek.com)
Google Metacreatures
These websites use Google or Yahoo APIs trying to broaden their functionality. Check them out.
XtraGoogle has a portal-like look showing most of the innumerable by now Google services.
YaGoohoo!gle combines Google and Yahoo in two side-by-side panes.
Send big files up to 1 GB for free
If you have a file that is too big for email (more than 10 MB), there is solution, YouSendIt.com lets you send files up to 1GB. You get a download link by e-mail, and even better - YouSendIt is free.
Source: PC Mag
Upload Movies or MP3 for Free
OurMedia.org woll host your multimedia for free, provided you share it with others.
BBC Radio Programs Available for Online Listening
BBC Radio 4 Listen Again page is a true internet treasure, if there is such thing. It contains most of the recent BBC programs which cover a variety of topics as wide as the world. The streaming Real player is required and, of course, the listening is free.
RSS via Email
If you are too lazy to use a RSS-aggregator, RMail is the "back-to-basics" option. Subscribe to RSS feeds and have them delivered to your email.
More options:
Bloglines - online RSS aggregator
Opera has a RSS reader embedded in the browser or you can download a Firefox plug-in
Stand-alone RSS readers (destined to disappear as most browsers will have RSS readers as part of them).
Thursday, April 28, 2005
Saturday, April 23, 2005
Bariatric Surgery Patient After the Roux-En-Y Operation
57 yo CF with PMH of morbid obesity is seen just after Roux-En-Y gastric bypass surgery (RYGB).
PMH:
Morbid obesity, HTN, GERD, Depression, OSA on CPAP, DM2, HPL, DJD
Medications:
Mavik, Metoprolol, Nexium, Zoloft, Zocor, ASA, Relafen, NPH insulin, Metformin
Physical examination:
Obese lady in NAD
VS 36.7-16-72-140/85 SpO2 96% 0n 5L
Chest: CTA (B)
CVS: Clear S1S2
Abdomen: surgical dressing
Extremities: no c/c/e
Where should this patient go after surgery - regular floor or ICU?
First, ask how long she had been on CPAP for OSA.
If more than 7 days and VSS, she can go to RMF.
If less than 7 days, she needs to go to the unit for an overnight stay.
What else should you do?
Check the CPAP settings. Most patients know the settings of their CPAP machine. Usually it is 5-20 cm H2O (not mm Hg).
If the patient does not know her CPAP setting, you can initially use a dynamic CPAP machine which adjusts the pressure automatically.
Always try to get the correct CPAP setting. To make a presumption is just like saying "hmmm...we do not know the Dig dose but let's try 0.25 mg..."
What should we do with all those pills she was taking before the surgery?
Restart the antidepressant and PPI.
Start SSI with Accuchecks qid.
Do not restart the NPH insulin, statin and BP medications automatically. Wait to see what this patient's PO intake will be.
Most patients have a significant weight loss after surgery and they may not need medications for their insulin resistance, HTN and hypercholesterolemia because these problems either resolve ot improve.
You cannot use extended release tablets because in the first few weeks they have to be crushed. Bariatric surgery patients are fed pureed diet for 2-3 weeks.
Incentive Spirometry
There is another key question to ask: How much do you do on the incentive spirometer?
The baseline value is determined prior to surgery. After the operation, the patient is expected to reach at least 30% of the baseline.
If the patient blew out 2000 cc on the spirometer before the surgery, she is are expected to reach 700 cc now. Most patients perform much better though.
Incentive spirometry is important to prevent atelectasis and then unnecessary work-up for fever.
Key Points of Interest After RYGB:
CPAP setting and duration of the treatment
Incentive Spirometry
Change in the medications
Diet
What did we learn from this case?
There is a list of 4 medical problems seen very commonly in bariatric patients: HTN, DM 2, DJD and depression.
After extubation, and before transferring the patient to the floor, make sure that she does not
have stridor due to glottic edema or wheezing/crackles due to pulmonary edema.
Incentive spirometry is essential in the postoperative period. If the patient did 2000 cc pre-op, they have to reach at least 30 percent of this after surgery (1000 cc is great).
References:
Patient Education for Incentive Spirometry - University of Utah Health Sciences Center
Incentive Spirometry - AARC Clinical Practice Guideline
Preventing respiratory problems after abdominal surgery - BMJ 1996, Tips from Other Journals - AFP
Obesity: Assessment and Management in Primary Care - AFP 06/01
The Risks of Bariatric Surgery - Other Perils of Overweight - NY Times 05/05
A case of gastric bypass surgery that went wrong. Struggling with Body Image During the Holidays - NPR 11/05
PMH:
Morbid obesity, HTN, GERD, Depression, OSA on CPAP, DM2, HPL, DJD
Medications:
Mavik, Metoprolol, Nexium, Zoloft, Zocor, ASA, Relafen, NPH insulin, Metformin
Physical examination:
Obese lady in NAD
VS 36.7-16-72-140/85 SpO2 96% 0n 5L
Chest: CTA (B)
CVS: Clear S1S2
Abdomen: surgical dressing
Extremities: no c/c/e
Where should this patient go after surgery - regular floor or ICU?
First, ask how long she had been on CPAP for OSA.
If more than 7 days and VSS, she can go to RMF.
If less than 7 days, she needs to go to the unit for an overnight stay.
What else should you do?
Check the CPAP settings. Most patients know the settings of their CPAP machine. Usually it is 5-20 cm H2O (not mm Hg).
If the patient does not know her CPAP setting, you can initially use a dynamic CPAP machine which adjusts the pressure automatically.
Always try to get the correct CPAP setting. To make a presumption is just like saying "hmmm...we do not know the Dig dose but let's try 0.25 mg..."
What should we do with all those pills she was taking before the surgery?
Restart the antidepressant and PPI.
Start SSI with Accuchecks qid.
Do not restart the NPH insulin, statin and BP medications automatically. Wait to see what this patient's PO intake will be.
Most patients have a significant weight loss after surgery and they may not need medications for their insulin resistance, HTN and hypercholesterolemia because these problems either resolve ot improve.
You cannot use extended release tablets because in the first few weeks they have to be crushed. Bariatric surgery patients are fed pureed diet for 2-3 weeks.
Incentive Spirometry
There is another key question to ask: How much do you do on the incentive spirometer?
The baseline value is determined prior to surgery. After the operation, the patient is expected to reach at least 30% of the baseline.
If the patient blew out 2000 cc on the spirometer before the surgery, she is are expected to reach 700 cc now. Most patients perform much better though.
Incentive spirometry is important to prevent atelectasis and then unnecessary work-up for fever.
Key Points of Interest After RYGB:
CPAP setting and duration of the treatment
Incentive Spirometry
Change in the medications
Diet
What did we learn from this case?
There is a list of 4 medical problems seen very commonly in bariatric patients: HTN, DM 2, DJD and depression.
After extubation, and before transferring the patient to the floor, make sure that she does not
have stridor due to glottic edema or wheezing/crackles due to pulmonary edema.
Incentive spirometry is essential in the postoperative period. If the patient did 2000 cc pre-op, they have to reach at least 30 percent of this after surgery (1000 cc is great).
References:
Patient Education for Incentive Spirometry - University of Utah Health Sciences Center
Incentive Spirometry - AARC Clinical Practice Guideline
Preventing respiratory problems after abdominal surgery - BMJ 1996, Tips from Other Journals - AFP
Obesity: Assessment and Management in Primary Care - AFP 06/01
The Risks of Bariatric Surgery - Other Perils of Overweight - NY Times 05/05
A case of gastric bypass surgery that went wrong. Struggling with Body Image During the Holidays - NPR 11/05
OSA, Sleep Study and CPAP settings
27 yo CM, morbidly obese is seen for preoperative evaluation for Roux-en-Y gastric bypass surgery. He has suffered from obesity for many years and has tried numerous weight-reduction programs with no success. His current weight is 395 pounds, and his height is 5 feet, 11 inches. He denies any symptoms of chest pain, palpitations, heart murmurs or irregular pulse. No history of orthopnea. He has exertional dyspnea. No history of asthma, emphysema or chronic cough. No history of smoking.
PMH:
Obesity, OSA (a sleep study was ordered), DJD, psoriasis
SH:
Denies any history of alcohol, tobacco or illicit drugs.
FH:
Father has OSA.
Medications:
Motrin PRN, HCTZ
Physical examination:
VS 36.8-16-84-133/85
Morbidly obese, in NAD
The rest of the examination is unremarkable.
EKG: NSR, HR 79, left axis.
What happened?
He had a sleep study which conformed the clinical suspicion of OSA. The recommended setting was CPAP 10 cm H2O QHS. The first step in treating OSA is to find the right CPAP setting. The second is to find the device that fits the patient and is tolerated. Nasal trumpets are tolerated best but they cannot deliver pressure higher than 10 cm H2O. The full face mask is the most effective device, delivering pressure up to 20 cm H20, but many patients experience claustrophobia, find it very uncomfortable, and for these reasons, do not use it.
Sleep Study Report
Weight (lbs) = 406
Height = 70
Study type: SPLIT NIGHT PSG
Indications: Loud snoring, excessive daytime sleepiness.
ESS = 6
PMH: morbid obesity
Medications: Ambien given for the test
He is undergoing preop evaluation for bariatric surgery
PROCEDURE
An overnight/daytime full montage split night polysomnography was performed, recording EEG, EOG, chin and leg EMG, EKG airflow, thoracic and abdominal effort, snoring via a microphone, pulse oximetry, body positioning and CPAP pressure.
SLEEP ARCHITECTURE=
Total recording time=395
sleep efficiency was=increased
Sleep efficiency (normal about 85%)=96
Sleep latency was=reduced
Sleep Latency in minutes (normal 15-20 min)=3
Sleep architecture revealed=reduced amounts of REM sleep
REM % of TST (normal=20% of TST)=0.5
REM latency was=REM was absent
(Normal REM latency 70-120 min)=66
REM rebound was seen on CPAP
RESPIRATORY SUMMARY:
At (cmH20) =0
L/min O2 =0
Baseline SpO2 %=97
Min SpO2 %=87
NREM AHI=109
REM AHI=240
Overall RDI=112
Overall AHI=110
Respiratory Index=2
Obstructive apneas=38
Central Apneas=0
Hypopneas=158
Respiratory Effort Related Arousals (RERAS)=4
SNORING DATA:
Snoring without CPAP (% of sleep time)=49
Snoring was reported as=loud
CPAP ANALYSIS:
CPAP titration was started at=5
CPAP/BiPAP final pressure=13
In this study the most adequate pressure was=10
Higher pressures =no significant benefit
IMPRESSION:
Obstructive Sleep Apnea with hypersomnia
OSA=severe
RECOMMENDATIONS:
Avoid sedatives, hypnotics and narcotics=unless sleep apnea treated.
CPAP/BIPAP cm H20=10.
Do not operate heavy machinery or drive=unless OSA/other sleep disorder treated
Weight reduction=to IBW
Heated humidifier=with CPAP
What happened next?
He has been on CPAP for 2 weeks and today he had a Roux-en-Y gastric bypass surgery 2 hours ago.
He has been on CPAP for more than one week, VS are stable and he can be transferred to RMF.
What did we learn from this case?
The most important parameter for diagnosing OSA is AHI (Apnea-Hypopnea Index). In healthy people AHI is less than 10.
If you have to choose just one number to diagnose OSA, choose AHI. As a single measurement AHI is comparable to the importance of RSBI in weaning and extubation. RSBI of less than 100 predicts the successful extubation of a ventilated patient in 85 percent of the cases.
This is a simple bedside evaluation for OSA:
Physical exam - just check two things:
-Neck size
The risk size for OSA is 17' for men, and 16' for women
-Look inside the patient's mouth: "Open your mouth please" and check the the Mallampati Score (MS)
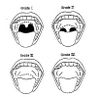
Mallampati Score (source: med.univ-rennes1.fr)
History:
-Epworth Sleepiness Scale (ESS), if more than 12, the patient is at high risk for OSA
References:
Obstructive Sleep Apnea-Hypopnea Syndrome - eMedicine
Snoring and Obstructive Sleep Apnea, Upper Airway Evaluation - eMedicine
Epworth Sleepiness Scale - University of Maryland, SMMC.com,
Treatment of Obstructive Sleep Apnea in Primary Care - AFP 02/04
Obstructive Sleep Apnea - AFP 11/99
Dr. Magboul Anesthesia page - MSN
Obstructive Sleep Apnea as a Risk Factor for Stroke and Death - NEJM 11/05
Continuous Positive Airway Pressure for Central Sleep Apnea and Heart Failure - NEJM 11/05
Sleep — A New Cardiovascular Frontier - NEJM Editorial 11/05
PMH:
Obesity, OSA (a sleep study was ordered), DJD, psoriasis
SH:
Denies any history of alcohol, tobacco or illicit drugs.
FH:
Father has OSA.
Medications:
Motrin PRN, HCTZ
Physical examination:
VS 36.8-16-84-133/85
Morbidly obese, in NAD
The rest of the examination is unremarkable.
EKG: NSR, HR 79, left axis.
What happened?
He had a sleep study which conformed the clinical suspicion of OSA. The recommended setting was CPAP 10 cm H2O QHS. The first step in treating OSA is to find the right CPAP setting. The second is to find the device that fits the patient and is tolerated. Nasal trumpets are tolerated best but they cannot deliver pressure higher than 10 cm H2O. The full face mask is the most effective device, delivering pressure up to 20 cm H20, but many patients experience claustrophobia, find it very uncomfortable, and for these reasons, do not use it.
Sleep Study Report
Weight (lbs) = 406
Height = 70
Study type: SPLIT NIGHT PSG
Indications: Loud snoring, excessive daytime sleepiness.
ESS = 6
PMH: morbid obesity
Medications: Ambien given for the test
He is undergoing preop evaluation for bariatric surgery
PROCEDURE
An overnight/daytime full montage split night polysomnography was performed, recording EEG, EOG, chin and leg EMG, EKG airflow, thoracic and abdominal effort, snoring via a microphone, pulse oximetry, body positioning and CPAP pressure.
SLEEP ARCHITECTURE=
Total recording time=395
sleep efficiency was=increased
Sleep efficiency (normal about 85%)=96
Sleep latency was=reduced
Sleep Latency in minutes (normal 15-20 min)=3
Sleep architecture revealed=reduced amounts of REM sleep
REM % of TST (normal=20% of TST)=0.5
REM latency was=REM was absent
(Normal REM latency 70-120 min)=66
REM rebound was seen on CPAP
RESPIRATORY SUMMARY:
At (cmH20) =0
L/min O2 =0
Baseline SpO2 %=97
Min SpO2 %=87
NREM AHI=109
REM AHI=240
Overall RDI=112
Overall AHI=110
Respiratory Index=2
Obstructive apneas=38
Central Apneas=0
Hypopneas=158
Respiratory Effort Related Arousals (RERAS)=4
SNORING DATA:
Snoring without CPAP (% of sleep time)=49
Snoring was reported as=loud
CPAP ANALYSIS:
CPAP titration was started at=5
CPAP/BiPAP final pressure=13
In this study the most adequate pressure was=10
Higher pressures =no significant benefit
IMPRESSION:
Obstructive Sleep Apnea with hypersomnia
OSA=severe
RECOMMENDATIONS:
Avoid sedatives, hypnotics and narcotics=unless sleep apnea treated.
CPAP/BIPAP cm H20=10.
Do not operate heavy machinery or drive=unless OSA/other sleep disorder treated
Weight reduction=to IBW
Heated humidifier=with CPAP
What happened next?
He has been on CPAP for 2 weeks and today he had a Roux-en-Y gastric bypass surgery 2 hours ago.
He has been on CPAP for more than one week, VS are stable and he can be transferred to RMF.
What did we learn from this case?
The most important parameter for diagnosing OSA is AHI (Apnea-Hypopnea Index). In healthy people AHI is less than 10.
If you have to choose just one number to diagnose OSA, choose AHI. As a single measurement AHI is comparable to the importance of RSBI in weaning and extubation. RSBI of less than 100 predicts the successful extubation of a ventilated patient in 85 percent of the cases.
This is a simple bedside evaluation for OSA:
Physical exam - just check two things:
-Neck size
The risk size for OSA is 17' for men, and 16' for women
-Look inside the patient's mouth: "Open your mouth please" and check the the Mallampati Score (MS)
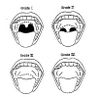
Mallampati Score (source: med.univ-rennes1.fr)
History:
-Epworth Sleepiness Scale (ESS), if more than 12, the patient is at high risk for OSA
References:
Obstructive Sleep Apnea-Hypopnea Syndrome - eMedicine
Snoring and Obstructive Sleep Apnea, Upper Airway Evaluation - eMedicine
Epworth Sleepiness Scale - University of Maryland, SMMC.com,
Treatment of Obstructive Sleep Apnea in Primary Care - AFP 02/04
Obstructive Sleep Apnea - AFP 11/99
Dr. Magboul Anesthesia page - MSN
Obstructive Sleep Apnea as a Risk Factor for Stroke and Death - NEJM 11/05
Continuous Positive Airway Pressure for Central Sleep Apnea and Heart Failure - NEJM 11/05
Sleep — A New Cardiovascular Frontier - NEJM Editorial 11/05
Right lung collapse in a ventilated patient due to mucus plug
32 yo AAF was admitted to the hospital with aspiration pneumonia and respiratory failure. She was not weanable from the ventilator and a tracheostomy was placed. The patient was admitted to an acute long-term care facility where she was following a chronic weraning protocol. While there, she had had a cardiorespiratory arrest and developed anoxic encephalopathy. The family insists on full code.
She is in ICU on vent. ABGs and CXRs show ARDS. Serial CXRs revealed worsening right lung collapse.

ABGs in ARDS
CXR


Right lung atelectasis with a shift of the mediastinum. ETT size 6 is too small to pass the bronschoscope for diagnosis and therapeutic suctioning.

Persistent atelectasis
CXR report:
Since yesterday, limited portable supine is the exam shows stable opaque right thorax mediastinal shift to the right, likely collapse of right lung with an endobronchial obstruction including underlying neoplasm considered as well as mucus plugging bronchogenic obstruction. Haziness of left mid and lower lung likely represents layering of left pleural effusion. Right cardiac border remains obscured.
What is the reason for the right lung opacification?
Mucus plug is the most likely cause for lung collapse in this patient.
DDx: CA (unlikely at this age)
What to do?
Bronchoscopy with mucus plug susctioning.
But first you have to check the size of the tracheostomy tube because the bronchoscope does not pass if the tube size is less than 8.
Her t-tube is 6. ENT consult was called and the t-tube was replaced with another one, size 8.
In the meantime, Mucomyst aerosol q 4 hr was started.
What happened?
Two hours after the t-tube was replaced and the tube was suctioned, the CXR showed a complete resolution of the right lung atelectasis. The oxygenation improved and the FiO2 was decreased. Mucomyst was stopped because it may act as an airway irritant on its own. A bronchoscopy was not needed.
CXR


Trachea was suctioned and the ETT was changed with a larger one, size 8. The removed ETT was filled with thick yellow-grey mucus. The follow-up CXR showed reexpansion of the right lung. See the close-up of the ETT, size 8 is the minimal size allowing the passage of a bronchoscope.
CXR report:
There is improved aeration of the right lung. There are infiltrates or atelectases in the both lungs with pleural effusions. There is again cardiomegaly with pulmonary venous hypertension and CHF. The life support device placement is unchanged.

ABGs show a decrease in the required FiO2 after the atelectasis resolved
Final diagnosis: Right lung collapse in a ventilated patient due to mucus plug
What did we learn from this case?
There are several causes for sudden deterioration of oxygenation of a ventilated patient:
-Pneumothorax
-Atelectasis
-Pulmonary edema
Atelectasis is often due to mucus plug and can be resolved by suctioning of the ETT.
In all cases of sudden deterioration, the patient needs a CXR immediately.
She is in ICU on vent. ABGs and CXRs show ARDS. Serial CXRs revealed worsening right lung collapse.

ABGs in ARDS
CXR


Right lung atelectasis with a shift of the mediastinum. ETT size 6 is too small to pass the bronschoscope for diagnosis and therapeutic suctioning.

Persistent atelectasis
CXR report:
Since yesterday, limited portable supine is the exam shows stable opaque right thorax mediastinal shift to the right, likely collapse of right lung with an endobronchial obstruction including underlying neoplasm considered as well as mucus plugging bronchogenic obstruction. Haziness of left mid and lower lung likely represents layering of left pleural effusion. Right cardiac border remains obscured.
What is the reason for the right lung opacification?
Mucus plug is the most likely cause for lung collapse in this patient.
DDx: CA (unlikely at this age)
What to do?
Bronchoscopy with mucus plug susctioning.
But first you have to check the size of the tracheostomy tube because the bronchoscope does not pass if the tube size is less than 8.
Her t-tube is 6. ENT consult was called and the t-tube was replaced with another one, size 8.
In the meantime, Mucomyst aerosol q 4 hr was started.
What happened?
Two hours after the t-tube was replaced and the tube was suctioned, the CXR showed a complete resolution of the right lung atelectasis. The oxygenation improved and the FiO2 was decreased. Mucomyst was stopped because it may act as an airway irritant on its own. A bronchoscopy was not needed.
CXR


Trachea was suctioned and the ETT was changed with a larger one, size 8. The removed ETT was filled with thick yellow-grey mucus. The follow-up CXR showed reexpansion of the right lung. See the close-up of the ETT, size 8 is the minimal size allowing the passage of a bronchoscope.
CXR report:
There is improved aeration of the right lung. There are infiltrates or atelectases in the both lungs with pleural effusions. There is again cardiomegaly with pulmonary venous hypertension and CHF. The life support device placement is unchanged.

ABGs show a decrease in the required FiO2 after the atelectasis resolved
Final diagnosis: Right lung collapse in a ventilated patient due to mucus plug
What did we learn from this case?
There are several causes for sudden deterioration of oxygenation of a ventilated patient:
-Pneumothorax
-Atelectasis
-Pulmonary edema
Atelectasis is often due to mucus plug and can be resolved by suctioning of the ETT.
In all cases of sudden deterioration, the patient needs a CXR immediately.
Respiratory Depression due to Opioid and Benzodiazepine Overdose
76 yo AAF with COPD was noted to be very lethargic by her family. She takes Vicodin for chronic back pain. On arrival in the ER, the patient is unresponsive. ABG is ordered.
PMH: COPD, LBP, DM2, HTN
Medications: HCTZ, aerosols, insulin, Vicodin, Ambien, ASA
Physical exam:
Obese lady who is visibly SOB and lethargic
Chest: diminished air entry (B)
CVS: Clear S1S2
Abdomen: Soft, NT, ND
Ext: no edema
Neuro: grossly nonfocal, lethargic
What do you think is going on?
Respiratory depression due to opioid and benzodiapine overdose.
She was taking Vicodin for chronic back pain and Ambien for sleep.
What tests would you order?
CBCD, CMP
ABG
CXR, EKG
CPP x 2 q 8 hr
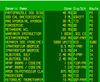
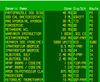
ABG (click to enlarge):

ABGs in opioid/BDZ overdose shows respiratory acidosis with compensatory metabolic alkalosis. The patient is a long-term COPD-er and this is the reason for the metabolic compensation. She retains HCO3 to compensate for the the chronic respiratory acidosis.
CXR showed COPD changes, EKG was unremarkable.
She was intubated because initially she was very lethargic and PaCO2 was 76.
Note that first she was on A/C and after a successful CPAP trial, she was extubated.

Urine toxic screen shows opiates and benzodiazepines
What happened?
Narcan is the drug of choice to be given to patients with opioid overdose.
She became more awake, the weaning parameters were good (see the picture), and she was successfully extubated.

Weaning parameters. The most important one is RSBI (rapid shallow breathing index). If RSBI is less than 100, the chances for successful extubation are more than 85%. Patients who fail the extubation attempt usually develop pulmonary edema or have stridor due to laryngeal edema from the endotracheal tube.
After the extubation, she had some wheezing and was treated for a few days with steroids.
During the hospital stay, a drop in her nocturnal SpO2 was noted. SpO2 was as low as 82% and dynamic CPAP had to be used.
We are virtually certain that she has OSA because she has most of the features - obesity, thick neck, snoring at night, sleepiness during the day, and nocturnal desaturation. She will need a formal sleep study as an outpatient to determine the correct BiPAP or CPAP settings.
Final diagnosis: Respiratory failure due to opioid and benzodiazepine overdose.
What did we learn from this case?
For COPD patients with chronic CO2 retention, it does not take much to push them over the top to acute respiratory acidosis.
Be careful when you prescribe opioids in COPD patients. It is better to avoid BDZ. Benadryl can be used as a sleeping aid instead of BDZ.
PMH: COPD, LBP, DM2, HTN
Medications: HCTZ, aerosols, insulin, Vicodin, Ambien, ASA
Physical exam:
Obese lady who is visibly SOB and lethargic
Chest: diminished air entry (B)
CVS: Clear S1S2
Abdomen: Soft, NT, ND
Ext: no edema
Neuro: grossly nonfocal, lethargic
What do you think is going on?
Respiratory depression due to opioid and benzodiapine overdose.
She was taking Vicodin for chronic back pain and Ambien for sleep.
What tests would you order?
CBCD, CMP
ABG
CXR, EKG
CPP x 2 q 8 hr
ABG (click to enlarge):

ABGs in opioid/BDZ overdose shows respiratory acidosis with compensatory metabolic alkalosis. The patient is a long-term COPD-er and this is the reason for the metabolic compensation. She retains HCO3 to compensate for the the chronic respiratory acidosis.
CXR showed COPD changes, EKG was unremarkable.
She was intubated because initially she was very lethargic and PaCO2 was 76.
Note that first she was on A/C and after a successful CPAP trial, she was extubated.

Urine toxic screen shows opiates and benzodiazepines
What happened?
Narcan is the drug of choice to be given to patients with opioid overdose.
She became more awake, the weaning parameters were good (see the picture), and she was successfully extubated.

Weaning parameters. The most important one is RSBI (rapid shallow breathing index). If RSBI is less than 100, the chances for successful extubation are more than 85%. Patients who fail the extubation attempt usually develop pulmonary edema or have stridor due to laryngeal edema from the endotracheal tube.
After the extubation, she had some wheezing and was treated for a few days with steroids.
During the hospital stay, a drop in her nocturnal SpO2 was noted. SpO2 was as low as 82% and dynamic CPAP had to be used.
We are virtually certain that she has OSA because she has most of the features - obesity, thick neck, snoring at night, sleepiness during the day, and nocturnal desaturation. She will need a formal sleep study as an outpatient to determine the correct BiPAP or CPAP settings.
Final diagnosis: Respiratory failure due to opioid and benzodiazepine overdose.
What did we learn from this case?
For COPD patients with chronic CO2 retention, it does not take much to push them over the top to acute respiratory acidosis.
Be careful when you prescribe opioids in COPD patients. It is better to avoid BDZ. Benadryl can be used as a sleeping aid instead of BDZ.
Respiratory Depression due to BDZ Overdose in a COPD Patient
54 yo CF with PMH of end-stage COPD fell and injured her left shoulder. She was taken to the nearest ER and received Toradol for pain. She became lethargic and was given Naloxone which made her agitated. She was given Ativan and shortly after that she became unresponsive.
PMH: COPD on home O2 - 5 l/min, DVT S/P IVC filter, HTN, heroin abuse on methadone now
Medications: Lasix, Prednisone, aerosols, Coumadin, Methadone
SH: Lives with her husband, smoker - 40 pck-yrs, heroin abuse in the past
Physical examination:
Thin lady, lethargic
VS 36.7-24-102-120/60
SpO2 90% on 5 L
Chest: decreased AE (B)
CVS: Clear S1S2
Abdomen: Soft, NDT, ND
Extremities: chronic stasis dermatitis (B)
What do you think is going on?
Respiratory depression from BDZ? Or oipoids?
What would you do?
She needs ABG stat.
Call a respiratory therapist because an intubation may be needed.
Order CBCD, CMP, CPP x 2 q 8 hr, EKG, CXR.


CBC and CMP; Urine toxic screen

ABGs in a patient with COPD and BDZ overdose
What happened?
Flumazenil 0.2 mg IV x 3 was given with an immediate response. BiPAP 16/6 was started and ABG was repeated.
Her mental status improved and she avoided intubation.
After 2 days treatment with Solu-Medrol and aerosols, she was discharged home.
Medications used
Final diagnosis: Respiratory depression due to BDZ in COPD
What did we learn from this case?
BDZ are contraindicated in COPD patients because they can induce a severe respiratory depression.
The antagonist drug of choice is Flumazenil. The beneficial effect is usually immediate (similar to Naloxone in opioid overdose). If the patient does not respond to repeated doses of Flumazenil, consider other diagnoses than BDZ overdose.
BiPAP can help avoid intubation in respiratory failure. Do not use it in unresponsive patients because of the aspiration risk. There should be a noticeable improvement in ABG within 30 min of BiPAP treatment.
PMH: COPD on home O2 - 5 l/min, DVT S/P IVC filter, HTN, heroin abuse on methadone now
Medications: Lasix, Prednisone, aerosols, Coumadin, Methadone
SH: Lives with her husband, smoker - 40 pck-yrs, heroin abuse in the past
Physical examination:
Thin lady, lethargic
VS 36.7-24-102-120/60
SpO2 90% on 5 L
Chest: decreased AE (B)
CVS: Clear S1S2
Abdomen: Soft, NDT, ND
Extremities: chronic stasis dermatitis (B)
What do you think is going on?
Respiratory depression from BDZ? Or oipoids?
What would you do?
She needs ABG stat.
Call a respiratory therapist because an intubation may be needed.
Order CBCD, CMP, CPP x 2 q 8 hr, EKG, CXR.


CBC and CMP; Urine toxic screen

ABGs in a patient with COPD and BDZ overdose
What happened?
Flumazenil 0.2 mg IV x 3 was given with an immediate response. BiPAP 16/6 was started and ABG was repeated.
Her mental status improved and she avoided intubation.
After 2 days treatment with Solu-Medrol and aerosols, she was discharged home.
Medications used
Final diagnosis: Respiratory depression due to BDZ in COPD
What did we learn from this case?
BDZ are contraindicated in COPD patients because they can induce a severe respiratory depression.
The antagonist drug of choice is Flumazenil. The beneficial effect is usually immediate (similar to Naloxone in opioid overdose). If the patient does not respond to repeated doses of Flumazenil, consider other diagnoses than BDZ overdose.
BiPAP can help avoid intubation in respiratory failure. Do not use it in unresponsive patients because of the aspiration risk. There should be a noticeable improvement in ABG within 30 min of BiPAP treatment.
Amiodarone-Induced Pulmonary Toxicity
57 yo AAM is admitted to the hospital with SOB for 7 days. He has leg edema which is getting progressively worse, to the point where his scrotum, penis and even his lower abdomen are now edematous. No CP or abdominal pain. He is morbidly obese and has difficulty ambulating, uses a wheelchair at home.
PMH: CHF, HTN, DM2, CAD, CRI, BPH, AFib, Gout, OA, OSA on home O2 3 L/min and CPAP
Medications: KCl, Coreg, Zocor, Flomax, Lasix, Clonidine, Percocet, Nifedipine XL, Humulin N, aerosols, Amiodarone
FMH: HTN
SH: negative
Physical examination:
VS 36.4-80-22-160/77
SpO2 94% on 3 L/min
Morbidly obese, appears mildly tachypneic
Chest: mild respiratory distress with RR 22, bibasilar rales
CVS: irregularly irregular rhythm
Abdomen: obese, soft, generalized anasarca with edema extending up to the level of his umbilicus. His penis and testicles are edematous. He has 2 to 3+ peripheral edema with bilateral Dome wraps on for management of stasis edema.

CXR showed pulmonary congestion.

CBC, CMP
Diagnosis:
Right-sided and left-sided CHF.
What happened?
He was started on Lasix and CPAP.
He was ruled out for AMI but he continued to be tachypneic and hypoxic.
What happened next?
Amiodarone-induced pulmonary toxicity was suspected.
The patient was diagnosed with AFib with RVR, difficult to control, approximately one year ago. He was started on Amiodarone 400 mg qd, decreased to 200 mg qd.
What are the tests of choice for Amiodarone-induced pulmonary toxicity?
High-resolution CT scan of the chest
PFT
DLCO




CT of the chest



High-resolution CT


High-resolution CT
CT of the chest report:
Nonspecific diffuse ground glass mosaic pattern of the lung parenchyma. There are bilateral linear scars or atelectases particularly into the lower lobes and right middle lobe.
Impression: Nonspecific ground glass mosaic pattern indicating interstitial lung disease.
Follow-up dedicated CT scan of the chest is recommended to confirm.
Final diagnosis: Amiodarone-induced pulmonary toxicity
What did we learn from this case?
Amiodarone-induced lung toxicity occurs in 6-15% of the patients treated. A drop of 15% in DLCO helps to make the diagnosis.
Toxicity occurs even at the lower Amiodarone doses like 200 mg qd.
Treatment is with a corticosteroid trial as with the other idiopathic interstitial lung diseases. There is no RCT proving that steroids are beneficial.
References:
Prescribing Amiodarone: An Evidence-Based Review of Clinical Indications. JAMA, 2007.
Pneumonitis and pulmonary fibrosis associated with amiodarone treatment: a possible complication of a new antiarrhythmic drug. This is the first report of Amiodarone-induced pulmonary toxicity. Circulation.org, 1982.
Amiodarone - Reevaluation of an Old Drug. Annals of Int Med.
Amiodarone-Induced Pulmonary Toxicity. NEJM Images.
Pulmonary Fibrosis, Idiopathic. eMedicine.
Amiodarone pulmonary toxicity. VH.org.
Amiodarone: Guidelines for Use and Monitoring. AFP 12/2003.
PMH: CHF, HTN, DM2, CAD, CRI, BPH, AFib, Gout, OA, OSA on home O2 3 L/min and CPAP
Medications: KCl, Coreg, Zocor, Flomax, Lasix, Clonidine, Percocet, Nifedipine XL, Humulin N, aerosols, Amiodarone
FMH: HTN
SH: negative
Physical examination:
VS 36.4-80-22-160/77
SpO2 94% on 3 L/min
Morbidly obese, appears mildly tachypneic
Chest: mild respiratory distress with RR 22, bibasilar rales
CVS: irregularly irregular rhythm
Abdomen: obese, soft, generalized anasarca with edema extending up to the level of his umbilicus. His penis and testicles are edematous. He has 2 to 3+ peripheral edema with bilateral Dome wraps on for management of stasis edema.

CXR showed pulmonary congestion.

CBC, CMP
Diagnosis:
Right-sided and left-sided CHF.
What happened?
He was started on Lasix and CPAP.
He was ruled out for AMI but he continued to be tachypneic and hypoxic.
What happened next?
Amiodarone-induced pulmonary toxicity was suspected.
The patient was diagnosed with AFib with RVR, difficult to control, approximately one year ago. He was started on Amiodarone 400 mg qd, decreased to 200 mg qd.
What are the tests of choice for Amiodarone-induced pulmonary toxicity?
High-resolution CT scan of the chest
PFT
DLCO




CT of the chest



High-resolution CT


High-resolution CT
CT of the chest report:
Nonspecific diffuse ground glass mosaic pattern of the lung parenchyma. There are bilateral linear scars or atelectases particularly into the lower lobes and right middle lobe.
Impression: Nonspecific ground glass mosaic pattern indicating interstitial lung disease.
Follow-up dedicated CT scan of the chest is recommended to confirm.
Final diagnosis: Amiodarone-induced pulmonary toxicity
What did we learn from this case?
Amiodarone-induced lung toxicity occurs in 6-15% of the patients treated. A drop of 15% in DLCO helps to make the diagnosis.
Toxicity occurs even at the lower Amiodarone doses like 200 mg qd.
Treatment is with a corticosteroid trial as with the other idiopathic interstitial lung diseases. There is no RCT proving that steroids are beneficial.
References:
Prescribing Amiodarone: An Evidence-Based Review of Clinical Indications. JAMA, 2007.
Pneumonitis and pulmonary fibrosis associated with amiodarone treatment: a possible complication of a new antiarrhythmic drug. This is the first report of Amiodarone-induced pulmonary toxicity. Circulation.org, 1982.
Amiodarone - Reevaluation of an Old Drug. Annals of Int Med.
Amiodarone-Induced Pulmonary Toxicity. NEJM Images.
Pulmonary Fibrosis, Idiopathic. eMedicine.
Amiodarone pulmonary toxicity. VH.org.
Amiodarone: Guidelines for Use and Monitoring. AFP 12/2003.
Pneumoconiosis or Sarcoidosis? Or Both?
52 yo AAM is admitted to the hospital with CC: SOB and wheezing for 4 days. He has cough productive of clear white sputum and denies any fever or chills. He has a life-long history of asthma and says that he is compliant with his asthma inhalers. The patient was also diagnosed with sarcoidosis several years ago. He had a bronchoscopy and biopsy at that time which "did not show cancer".
PMH: Asthma/COPD, Sarcoidosis, HTN
Medications: Advair, inhalers, Lisinopril, HCTZ
SH: Former smoker
Physical examination:
VS 36.4-20-82-140/82
SpO2 98% on RA
Chest: decreased AE (B), wheezing (B)
CVS: Clear S1S2
Abdomen: Soft, NT, ND
Extremities: no c/c/e
What do you think is going on?
A typical asthma exacerbation?
Sarcoidosis flare-up?
Pneumonia?
Or something else?
What tests would you order?
CXR
CBCD, CMP
Sputum Gram stain, C+S
CXR


CXR two years ago. Close-up of the RLL.
CXR report: Since 2 years ago, limited portable upright view shows stable partially calcified hilar lymph nodes, pleural thickening of right minor fissure, the normal size heart. Previously demonstrated retrocardiac hiatus hernia is partly seen as a double density through the heart.


CXR on this admission; lateral CXR; report
He also had a CT scan of the chest which showed diffuse ground glass pattern.



CT chest two years ago



CT chest two years ago
CT report:
Findings: There is a calcified left periaortic lymph node. Calcified mediastinal nodes are also noted. These findings are likely due to remote granulomatous. There is a large hiatal hernia.
Lung windows show COPD. Scarring is noted in the right lung base. Increased interstitial markings are seen in the medial right lung base possibly due to chronic change
There is infiltrate extending from the right hilum to the right lateral chest wall. Similar but less extensive infiltrate extends from the left hilum to the left lateral chest wall. Mild right hilar adenopathy is noted.
Impression:
1. Mild right hilar adenopathy with bilateral perihilar infiltrates right more extensive than left extending to the periphery.
2. Signs of remote granulomatous disease
3. Large hiatal hernia
4. Nonspecific left upper lobe nodule. Follow-up CT in four months is recommended to document stability
5. Increased interstitial markings in the lung bases especially medial right lung base. These could be chronic and possibly related to scarring.





CT during this admission
CT chest report:
Since 2 years ago, again seen are enlarged mediastinal and hilar nodes some with calcifications. There is again a large hiatal hernia. There are enlarged bilateral pulmonary arteries creating the perihilar density seen on chest x-ray. Again seen are scars into both lung bases and infiltrates or atelectases/scars into the right middle and lower lobes. There is unchanged nonspecific ground glass parenchymal pattern in the left upper lobe. There is again diffuse haziness of the right lung. There are bilateral air cysts. There are bilateral upper lobe nodules which are stable. Again seen is bilateral pleural thickening right side greater than the left with fine nodular peripheral irregularity right side greater than the left.
Impression: Unchanged enlarged mediastinal and hilar nodes some with calcifications. New mildly enlarged retrocrural node.
Infiltrate, scar, atelectasis in the right middle and lower lobes with additional pulmonary parenchymal scars particularly in the lung bases. Unchanged mild pleural thickening which can be secondary to scar. Stable upper lobe nodules.
What did we miss when collecting the history?
Occupational exposure. Always ask about the former or current jobs when doing H&P for a patient with chronic lung disease.
As Osler said, in 80 percent of the time, the patient will give you the diagnosis if you ask the right questions. You may not even need the physical examination (but you always have to do it).
When asked what he worked before, this patient said he worked in a foundry for 3 years (occupational exposure to silica dust).
His previous computer records were reviewed carefully and he indeed had a lung biopsy. The problem was that the biopsy was not diagnostic for sarcoidosis. He had some of the features of the active disease, like elevated high ACE level but lacked some of the others like increased calcium.

Biopsy report
What happened?
He was started on Solu-Medrol 30 mg IV q 6 hr and aerosols q 4 hr. Gradually his symptoms resolved and he was discharged home. PPD was negative. The patient has a marked mediastinal lymphadenopathy which is not seen in pneumoconiosis and can be a feature of sarcoidosis. Lymphoma is is unlikely with such protracted disease course spanning several years. A second bronchoscopy with lymph node biopsy will be scheduled.
Final diagnosis: Pneumoconiosis and Suspected Sarcoidosis
What did we learn from this case?
Always collect occupational exposure history in patients with chronic lung disease. Do not be fooled by the "known history of" phrase because often when you look at the records, you will notice that the grounds for the particular diagnosis were not that firm.
What is a foundry?
An establishment where metal is melted and poured into molds. The molds are covered with sand from inside and then the heated metal is poured in. The sand evaporates from the heat and the air is filled with silica particles. After the metal cast cools of, its surface is still rough from the remaining silica particles and has to be smoothened. During this process there is even higher concentration of silica in the air.
All these occupational factors may lead to development of silicosis in foundry workers.
How are the pneumoconioses diagnosed?
By occupational history and CXR.
There is a classification for grading the severity of pneumoconioses - the PQRSTU system.
The PQRSTU System
The CXR shadow due to pneumoconioses are described as round or linear. The round shadows are graded in size from P (smallest) to R (largest). The linear shadows are graded from T (smallest) to U (largest).
This PQRSTU system reminds us of the PQRSTU nomenclature used to describe the different elements of the electrocardiogram.
PMH: Asthma/COPD, Sarcoidosis, HTN
Medications: Advair, inhalers, Lisinopril, HCTZ
SH: Former smoker
Physical examination:
VS 36.4-20-82-140/82
SpO2 98% on RA
Chest: decreased AE (B), wheezing (B)
CVS: Clear S1S2
Abdomen: Soft, NT, ND
Extremities: no c/c/e
What do you think is going on?
A typical asthma exacerbation?
Sarcoidosis flare-up?
Pneumonia?
Or something else?
What tests would you order?
CXR
CBCD, CMP
Sputum Gram stain, C+S
CXR


CXR two years ago. Close-up of the RLL.
CXR report: Since 2 years ago, limited portable upright view shows stable partially calcified hilar lymph nodes, pleural thickening of right minor fissure, the normal size heart. Previously demonstrated retrocardiac hiatus hernia is partly seen as a double density through the heart.


CXR on this admission; lateral CXR; report
He also had a CT scan of the chest which showed diffuse ground glass pattern.



CT chest two years ago



CT chest two years ago
CT report:
Findings: There is a calcified left periaortic lymph node. Calcified mediastinal nodes are also noted. These findings are likely due to remote granulomatous. There is a large hiatal hernia.
Lung windows show COPD. Scarring is noted in the right lung base. Increased interstitial markings are seen in the medial right lung base possibly due to chronic change
There is infiltrate extending from the right hilum to the right lateral chest wall. Similar but less extensive infiltrate extends from the left hilum to the left lateral chest wall. Mild right hilar adenopathy is noted.
Impression:
1. Mild right hilar adenopathy with bilateral perihilar infiltrates right more extensive than left extending to the periphery.
2. Signs of remote granulomatous disease
3. Large hiatal hernia
4. Nonspecific left upper lobe nodule. Follow-up CT in four months is recommended to document stability
5. Increased interstitial markings in the lung bases especially medial right lung base. These could be chronic and possibly related to scarring.





CT during this admission
CT chest report:
Since 2 years ago, again seen are enlarged mediastinal and hilar nodes some with calcifications. There is again a large hiatal hernia. There are enlarged bilateral pulmonary arteries creating the perihilar density seen on chest x-ray. Again seen are scars into both lung bases and infiltrates or atelectases/scars into the right middle and lower lobes. There is unchanged nonspecific ground glass parenchymal pattern in the left upper lobe. There is again diffuse haziness of the right lung. There are bilateral air cysts. There are bilateral upper lobe nodules which are stable. Again seen is bilateral pleural thickening right side greater than the left with fine nodular peripheral irregularity right side greater than the left.
Impression: Unchanged enlarged mediastinal and hilar nodes some with calcifications. New mildly enlarged retrocrural node.
Infiltrate, scar, atelectasis in the right middle and lower lobes with additional pulmonary parenchymal scars particularly in the lung bases. Unchanged mild pleural thickening which can be secondary to scar. Stable upper lobe nodules.
What did we miss when collecting the history?
Occupational exposure. Always ask about the former or current jobs when doing H&P for a patient with chronic lung disease.
As Osler said, in 80 percent of the time, the patient will give you the diagnosis if you ask the right questions. You may not even need the physical examination (but you always have to do it).
When asked what he worked before, this patient said he worked in a foundry for 3 years (occupational exposure to silica dust).
His previous computer records were reviewed carefully and he indeed had a lung biopsy. The problem was that the biopsy was not diagnostic for sarcoidosis. He had some of the features of the active disease, like elevated high ACE level but lacked some of the others like increased calcium.

Biopsy report
What happened?
He was started on Solu-Medrol 30 mg IV q 6 hr and aerosols q 4 hr. Gradually his symptoms resolved and he was discharged home. PPD was negative. The patient has a marked mediastinal lymphadenopathy which is not seen in pneumoconiosis and can be a feature of sarcoidosis. Lymphoma is is unlikely with such protracted disease course spanning several years. A second bronchoscopy with lymph node biopsy will be scheduled.
Final diagnosis: Pneumoconiosis and Suspected Sarcoidosis
What did we learn from this case?
Always collect occupational exposure history in patients with chronic lung disease. Do not be fooled by the "known history of" phrase because often when you look at the records, you will notice that the grounds for the particular diagnosis were not that firm.
What is a foundry?
An establishment where metal is melted and poured into molds. The molds are covered with sand from inside and then the heated metal is poured in. The sand evaporates from the heat and the air is filled with silica particles. After the metal cast cools of, its surface is still rough from the remaining silica particles and has to be smoothened. During this process there is even higher concentration of silica in the air.
All these occupational factors may lead to development of silicosis in foundry workers.
How are the pneumoconioses diagnosed?
By occupational history and CXR.
There is a classification for grading the severity of pneumoconioses - the PQRSTU system.
The PQRSTU System
The CXR shadow due to pneumoconioses are described as round or linear. The round shadows are graded in size from P (smallest) to R (largest). The linear shadows are graded from T (smallest) to U (largest).
This PQRSTU system reminds us of the PQRSTU nomenclature used to describe the different elements of the electrocardiogram.
Acrocyanosis in Pickwickian Syndrome
71 yo CM is admitted to the hospital with CC: SOB for 3 weeks. The patient is on home O2 and CPAP and despite using aerosols and his CPAP machine, SOB is getting worse. One week prior to admission he found that his oxygen machine was not working. The patient had also noticed that his hands and feet were getting bluish in color for the past two weeks. He was at his physician's office where he was found to have SpO2 of 70% and hence was advised to be admitted for further management. The patient denied fever, chills and cough. No history of CP or palpitations.
PMH: HTN, DM 2, COPD. Atrial fibrillation, OSA on CPAP 13 cm H2O and 5 L oxygen, pulmonary hypertension, CHF, CRI, Obesity
The patient had a sleep study one year ago which confirmed severe OSA. He had a 2-D echo at the same time which revealed moderate to severe pulmonary hypertension (70 mmHg), EF 40% to 45%.

2D Echo showed pulmonary hypertension with a PA pressure of 70 mm Hg
Medications: Actos, Amaryl, verapamil, Lasix, Coumadin, Flonase
SH: 50-pack-year history of smoking. He quit four years ago. He denies drinking alcohol or using illicit drugs.
Physical examination:
Obese man, dyspneic at rest.
VS 36.4-108-20-109/72
SpO2 85% to 88% on 5 L nasal cannula
Lungs: Decreased air entry bilaterally. No wheeze or crackles
CVS: Irregular rhythm
Abdomen: obese, protuberant
Extremities: 2+ pedal edema with bilateral chronic stasis changes. Skin of the fingers and toes is cyanotic and cold.




Acrocyanosis in a patient with polycythemia and hypoxemia

Cyanosis of the lips and tongue
EKG revealed atrial fibrillation, rate controlled, a low amplitude base and no acute ischemic changes.

CBD shows polycythemia due to persistent hypoxemia

CXR report

ABGs in Pickwickian syndrome
What happened?
He was started on CPAP with a pressure of 13 cm of water with oxygen titrated for a pulse oximetry of more than 94%.
The patient was also started on IV steroids and IV Lasix. He was advised to be on oxygen throughout the day with CPAP at night. The cyanosis in the extremities gradually resolved.
He was discharged to a transitional care unit.
Final diagnosis: End-stage respiratory failure. Cor pulmonale due to COPD, Pickwickian syndrome, OSA.
PMH: HTN, DM 2, COPD. Atrial fibrillation, OSA on CPAP 13 cm H2O and 5 L oxygen, pulmonary hypertension, CHF, CRI, Obesity
The patient had a sleep study one year ago which confirmed severe OSA. He had a 2-D echo at the same time which revealed moderate to severe pulmonary hypertension (70 mmHg), EF 40% to 45%.

2D Echo showed pulmonary hypertension with a PA pressure of 70 mm Hg
Medications: Actos, Amaryl, verapamil, Lasix, Coumadin, Flonase
SH: 50-pack-year history of smoking. He quit four years ago. He denies drinking alcohol or using illicit drugs.
Physical examination:
Obese man, dyspneic at rest.
VS 36.4-108-20-109/72
SpO2 85% to 88% on 5 L nasal cannula
Lungs: Decreased air entry bilaterally. No wheeze or crackles
CVS: Irregular rhythm
Abdomen: obese, protuberant
Extremities: 2+ pedal edema with bilateral chronic stasis changes. Skin of the fingers and toes is cyanotic and cold.




Acrocyanosis in a patient with polycythemia and hypoxemia

Cyanosis of the lips and tongue
EKG revealed atrial fibrillation, rate controlled, a low amplitude base and no acute ischemic changes.

CBD shows polycythemia due to persistent hypoxemia

CXR report

ABGs in Pickwickian syndrome
What happened?
He was started on CPAP with a pressure of 13 cm of water with oxygen titrated for a pulse oximetry of more than 94%.
The patient was also started on IV steroids and IV Lasix. He was advised to be on oxygen throughout the day with CPAP at night. The cyanosis in the extremities gradually resolved.
He was discharged to a transitional care unit.
Final diagnosis: End-stage respiratory failure. Cor pulmonale due to COPD, Pickwickian syndrome, OSA.
Subscribe to:
Posts (Atom)